
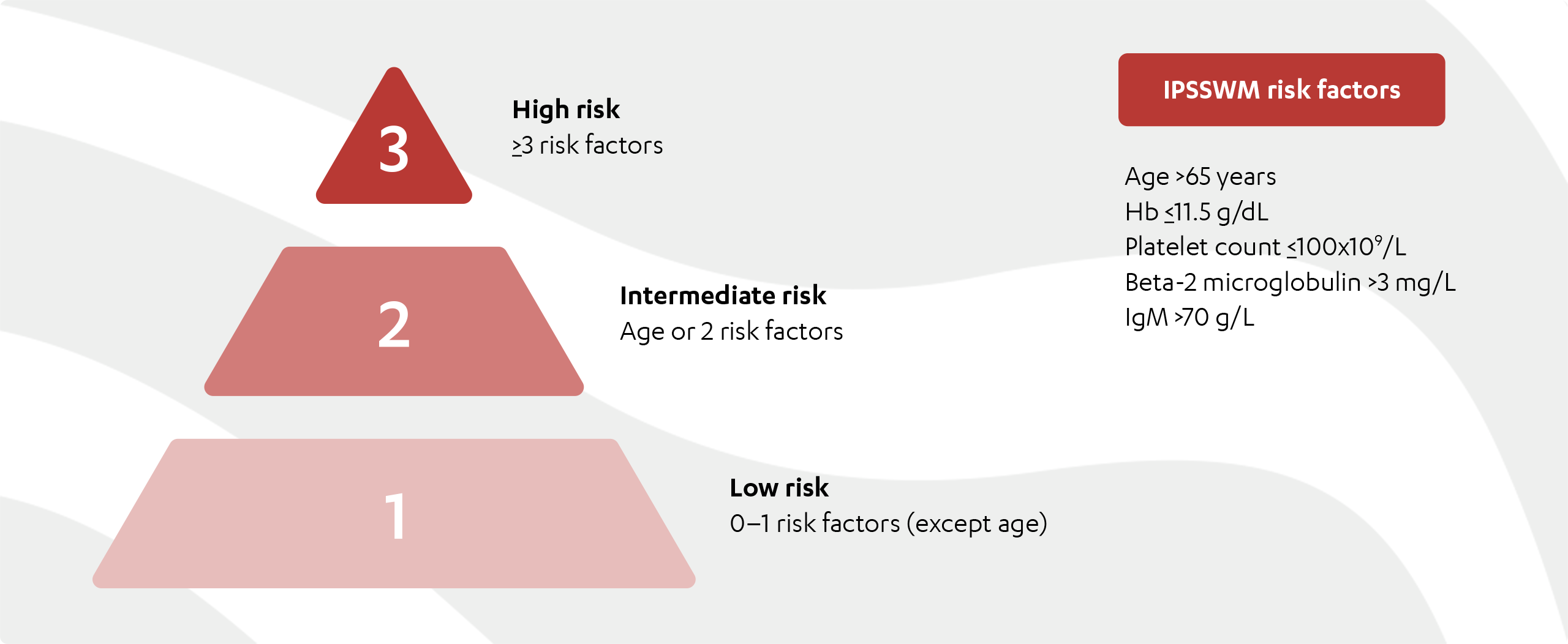
IPSSWM=International Prognostic Scoring System for WM; IgM=immunoglobulin M; Hb=hemoglobin.
Adapted from Morel P, et al.
ADDITIONAL TESTS
Additional work-up is often based on symptomatic presentation and laboratory findings that can indicate the need for treatment initiation (Table 1).2
| Symptom / clinical presentation | Test |
|---|---|
| Older adults | Frailty assessment |
| Hyperviscosity syndrome (symptoms include headaches, visual disturbances, confusion, vertigo, shortness of breath, epistaxis) | Serum viscosity
Retinal examination |
| Anemia with hemolysis | Cryoglobulins
Cold agglutinin titre |
| Unexpected clinical bleeding or bruising | von Willebrand disease (VWD) testing |
| Sensory peripheral neuropathy | Myelin-associated glycoprotein antibodies (serum anti-MAGs)
Consider specialist neurological evaluation |
| Motor neuropathy | Consider anti-ganglioside M1 (GM1) antibodies |
| Amyloidosis should be suspected in patients presenting with: nephrotic syndrome, axonal neuropathy, or unexplained cardiac problems | Fat biopsy and/or evaluation of the bone marrow biopsy with Congo red |
Adapted with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Waldenström Macroglobulinemia/Lymphoplasmatic Lymphoma V.2.2022 – December 7, 2021 © 2022 National Comprehensive Cancer Network, Inc. All rights reserved. The NCCN Guidelines® and illustrations herein may not be reproduced in any form for any purpose without the express written permission of the NCCN. To view the most recent and complete version of the NCCN Guidelines, go online to NCCN.org. The NCCN Guidelines are a work in progress that may be refined as often as new significant data becomes available. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
TO TREAT OR NOT TO TREAT?

According to the National Comprehensive Cancer Network® (NCCN®), treatment should be initiated only in WM patients who are symptomatic, and when it has been confirmed that their symptoms are not related to or caused by comorbidities.2
Studies have shown that patients with low Hb levels, high lymphoplasmacytic cell infiltration, IgM flare and high beta-2 microglobulin levels may be at higher risk for development of symptomatic WM.4,5 However patients may be asymptomatic for 5–10 years and can be managed with a “watch and wait” approach, without treatment.4
High level of monoclonal IgM alone should not be considered an indication to start treatment.2
Symptomatic hyperviscosity requires immediate disease control. Plasmapheresis should be used immediately in such patients, followed by the initiation of suitable systemic treatment as soon as possible.2
For the most common indications for treatment initiation, visit the “I can identify” page.
References:
- Morel P, et al. International prognostic scoring system for Waldenström Macroglobulinemia. Blood 2009;113(18):4163–4170.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Waldenström Macroglobulinemia/Lymphoplasmatic Lymphoma V.2.2022 – December 7, 2021 © National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Accessed March 4, 2022. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
- Leukemia & Lymphoma Society. Waldenström Macroglobulinemia facts. Available at: https://www.llscanada.org/sites/default/files/file_assets/FS20_Waldenstrom_M%20FINAL%206.15.pdf. Accessed August 24, 2021.
- Garcia-Sanz R, et al. Waldenström Macroglobulinaemia: presenting features and outcome in a series with 217 cases. Br J Haematol 2001;115:575–582.
- Kyle RA, et al. Progression in smoldering Waldenström Macroglobulinemia: long-term results. Blood 2012;119:4462–4466.
IgM=immunoglobulin M; Hb=hemoglobin; IPSSWM=International Prognostic Scoring System for WM; MAG=myelin-associated glycoprotein


