Figure 1. MCL DIAGNOSIS AND WORK-UP PATHWAY1
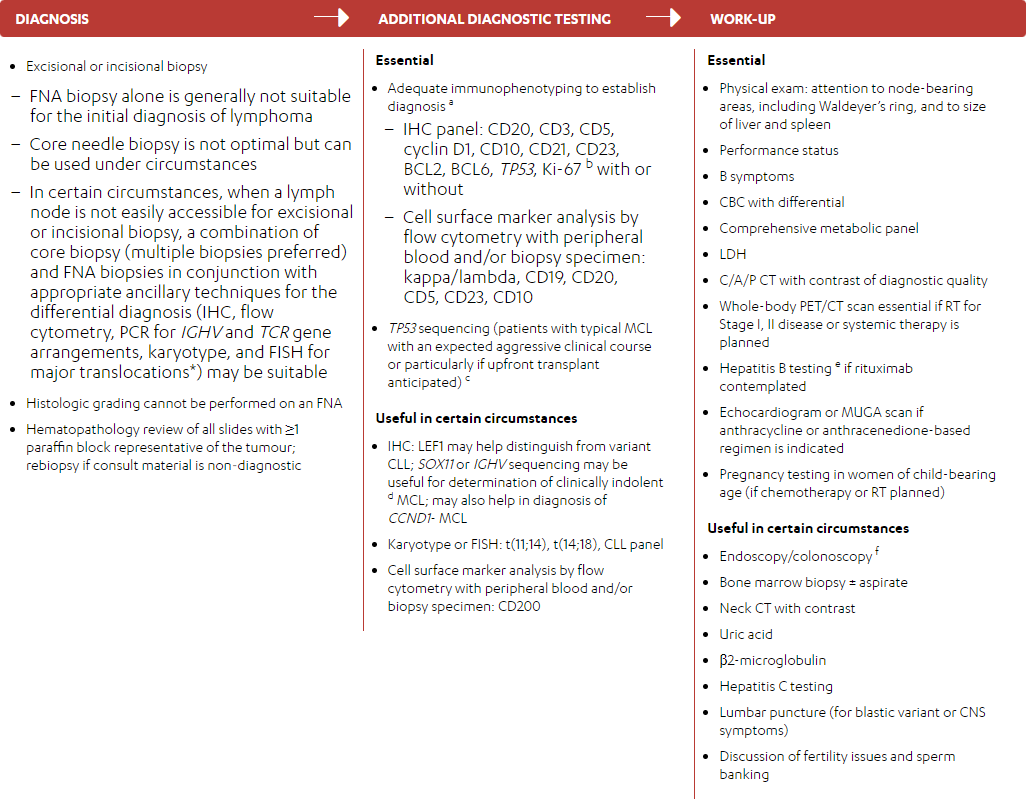
- Excisional or incisional biopsy
– FNA biopsy alone is generally not suitable for the initial diagnosis of lymphoma
– Core needle biopsy is not optimal but can be used under circumstances
– In certain circumstances, when a lymph node is not easily accessible for excisional or incisional biopsy, a combination of core biopsy (multiple biopsies preferred) and FNA biopsies in conjunction with appropriate ancillary techniques for the differential diagnosis (IHC, flow cytometry, PCR for IGHV and TCR gene arrangements, karyotype, and FISH for major translocations*) may be suitable
- Histologic grading cannot be performed on an FNA
- Hematopathology review of all slides with ≥1 paraffin block representative of the tumour; rebiopsy if consult material is non‑diagnostic
ADDITIONAL DIAGNOSTIC TESTING
-
Essential
- Adequate immunophenotyping to establish diagnosisa
– IHC panel: CD20, CD3, CD5, cyclin D1, CD10, CD21, CD23, BCL2, BCL6, TP53, SOX11, Ki-67 b with or without
– Cell surface marker analysis by flow cytometry with peripheral blood and/or biopsy specimen: kappa/lambda, CD19, CD20, CD5, CD23, CD10, CD200
– TP53 sequencingcc
- IHC: LEF1 may help distinguish from variant CLL; SOX11 or IGHV sequencing may be useful for determination of clinically indolentd MCL; may also help in diagnosis of CCND1- MCL
- Karyotype or FISH: t(11;14), t(14;18), CLL panel
- Cell surface marker analysis by flow cytometry with peripheral blood and/or biopsy specimen: CD200
- Adequate immunophenotyping to establish diagnosisa
WORK-UP
-
Essential
- Physical exam: attention to node-bearing areas, including Waldeyer’s ring, and to size of liver and spleen
- Performance status
- B symptoms
- CBC with differential
- Comprehensive metabolic panel
- LDH
- C/A/P CT with contrast of diagnostic quality
- Whole-body PET/CT scan essential if RT for Stage I, II disease or systemic therapy is planned
- Hepatitis B testinge if rituximab contemplated
- Echocardiogram or MUGA scan if anthracycline or anthracenedione-based regimen is indicated
- Pregnancy testing in women of child-bearing age (if chemotherapy or RT planned)
- Endoscopy/colonoscopyf
- Bone marrow biopsy ± aspirate
- Neck CT with contrast
- Uric acid
- beta-2 microglobulin
- Hepatitis C testing
- Lumbar puncture (for blastic variant or CNS symptoms)
- Discussion of fertility issues and sperm banking
FNA=fine needle aspiration; IHC=immunohistochemistry; PCR=polymerase chain reaction; IGHV=immunoglobin heavy chain variable; TCR=T-cell receptor; FISH=fluorescent in situ hybridization; LEF1=lymphoid enhancer-binding factor 1; CLL=chronic lymphocytic leukemia; CCND1=cyclin D1; CBC=complete blood count; LDH=lactate dehydrogenase; C/A/P=chest/abdominal/pelvic; CT=computerized tomography; PET=positron emission tomography; RT=radiotherapy; MUGA=multigated acquisition; CNS=central nervous system.
* If a high suspicion of a clonal process remains and other techniques have not resulted in a clear identification of a clonal process, then next-generation sequencing (NGS) can be used.
- Typical immunophenotype: CD5+, CD20+, CD43+, CD23-/+, cyclin D1+, CD10-/+. Note: Some cases of MCL may be CD5- or CD23+. If the diagnosis is suspected, cyclin D1 staining or FISH for t(11;14) should be done. There are rare cases of CCND1- MCL (<5%) with an otherwise typical immunophenotype.
- Ki-67 proliferation fraction of <30% in lymph nodes is associated with a more favourable prognosis.
- TP53 mutation has been associated with poor prognosis in patients treated with conventional therapy, including transplant. Clinical trial is strongly suggested for these patients. TP53 by IHC is not a proven surrogate for TP53 mutation status or del(17p) status.
- Most common biomarker for indolent disease: SOX11- [IGHV-mutated]. Typical clinical presentation: leukemic non-nodal CLL-like with splenomegaly, low tumour burden, Ki-67 proliferation fraction <10%.
- Hepatitis B testing is indicated because of the risk of reactivation with immunotherapy + chemotherapy. Tests include hepatitis B surface antigen and core antibody for a patient with no risk factors. For patients with risk factors or previous history of hepatitis B, add e-antigen. If positive, check viral load and consider consult with gastroenterologist.
- Essential for confirmation of Stage I–II disease.
Adapted with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for B-Cell Lymphomas V.1.2022 – March 2, 2022. © 2022 National Comprehensive Cancer Network, Inc. All rights reserved. The NCCN Guidelines® and illustrations herein may not be reproduced in any form for any purpose without the express written permission of the NCCN. To view the most recent and complete version of the NCCN Guidelines, go online to NCCN.org. The NCCN Guidelines are a work in progress that may be refined as often as new significant data becomes available. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
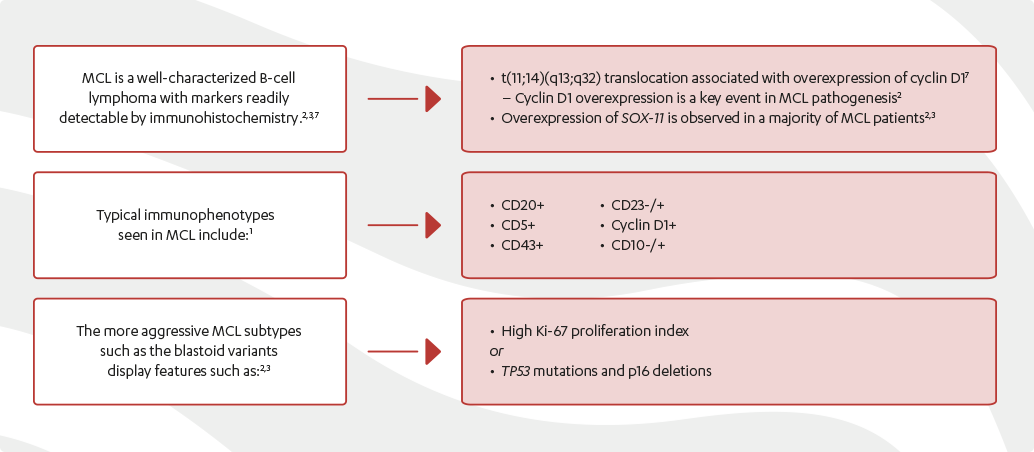
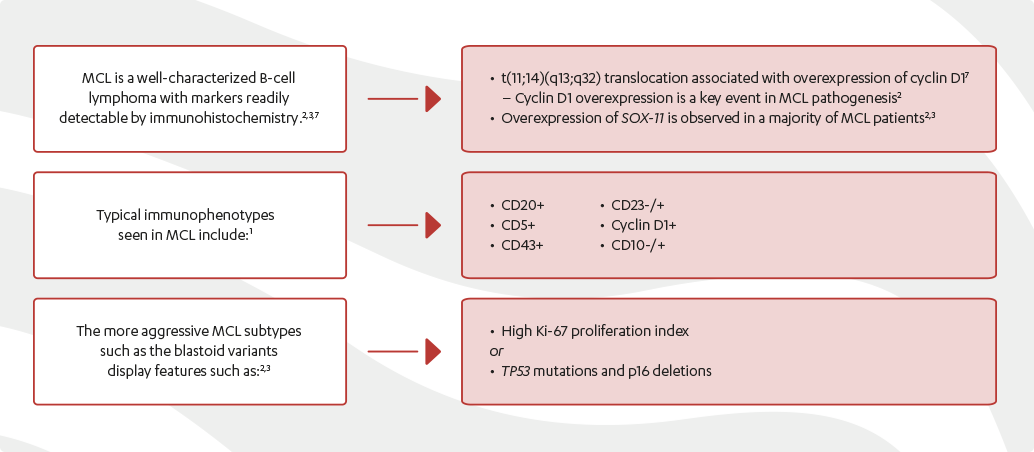
TYPES OF MCL
Conventional MCL (70−80%)2
Symptomatic lymph adenopathy or symptomatic extra-nodal disease requiring systemic therapy.
Smouldering nodal/extra-nodal MCL and asymptomatic purely leukemic non-blastoid MCL (10−20%)2
A “watch and wait” strategy should be considered for patients with asymptomatic, low MIPI or elderly patients due to the unfavourable prognosis and the limited efficacy with standard therapy (i.e., does not appear to cure) in patients with MCL.2,3
THE MCL DIAGNOSTIC PROCESS
A diagnosis of MCL requires histopathological confirmation of lymph node infiltration. A part, or all, of an easily accessible, enlarged lymph node will be removed.4–6
The histological report should give the diagnosis according to the World Health Organization (WHO) classification and Ki-67, a proliferation marker, as the most established histomorphological risk factor.6
Most tumours have a classic structure of small−medium-sized cells with irregular nuclei. However, the malignant lymphocytes may present in a variety of forms.6
Immunophenotyping using flow cytometry has become an integral part in the subclassification of B-cell lymphomas (Figure 2).7
BCL2=B-cell lymphoma 2.
The MCL subtypes present with different clinical pictures.2
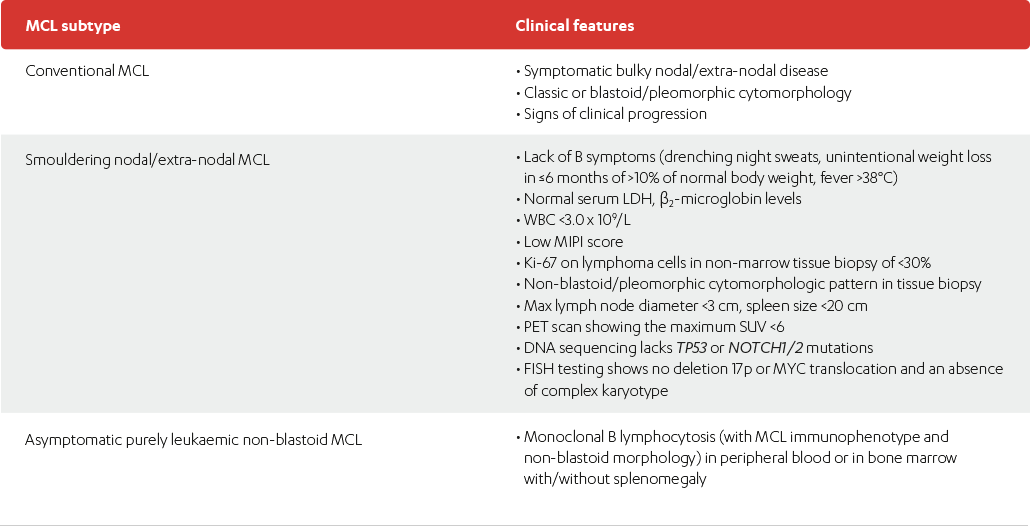
| MCL subtype | Clinical features |
|---|---|
| Conventional MCL |
|
| Smouldering nodal/extra-nodal MCL |
|
| Asymptomatic purely leukaemic non-blastoid MCL |
|
Adapted from Jain P and Wang M, 2019.
LDH=lactate dehydrogenase; WBC=white blood cell count; MIPI=mantle cell lymphoma international
prognostic index; PET=positron emission tomography; SUV=standardized uptake value; FISH=fluorescent
in situ hybridization.
References:
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for B-Cell Lymphomas V.1.2022 – March 2, 2022. © National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Accessed March 4, 2022. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
- Jain P and Wang M. Mantle cell lymphoma: 2019 update on the diagnosis, pathogenesis, prognostication, and management. Am J Hematol 2019;94:710–25.
- Vose J. Mantle cell lymphoma: 2017 update on diagnosis, risk-stratification, and clinical management. Am J Hematol 2017;92:806–13.
- Leukemia & Lymphoma Society. Mantle cell lymphoma facts. Available at: https://www.llscanada.org/sites/default/files/National/CANADA/Pdf/InfoBooklets/FS4_MCL_2018_FINAL.pdf. Accessed August 24, 2021.
- National Organization for Rare Disorders (NORD). Mantle cell lymphoma: General discussion. Accessed November 28, 2020, at: https://rarediseases.org/rare-diseases/mantle-cell-lymphoma/.
- Dreyling M, et al. Newly diagnosed and relapsed mantle cell lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2017;28(S4):iv62–iv71.
- Aqil B, et al. Immunophenotypic Variations in Mantle Cell Lymphoma and Their Impact on Clinical Behavior and Outcome. Arch Pathol Lab Med 2018;142(10):1268–74.
- McKay P, et al. A British Society for haematology good practice paper on the diagnosis and investigation of patients with mantle cell lymphoma. British Journal of Haematology 2018;182:63–70.