RISK STRATIFICATION AND PROGNOSIS
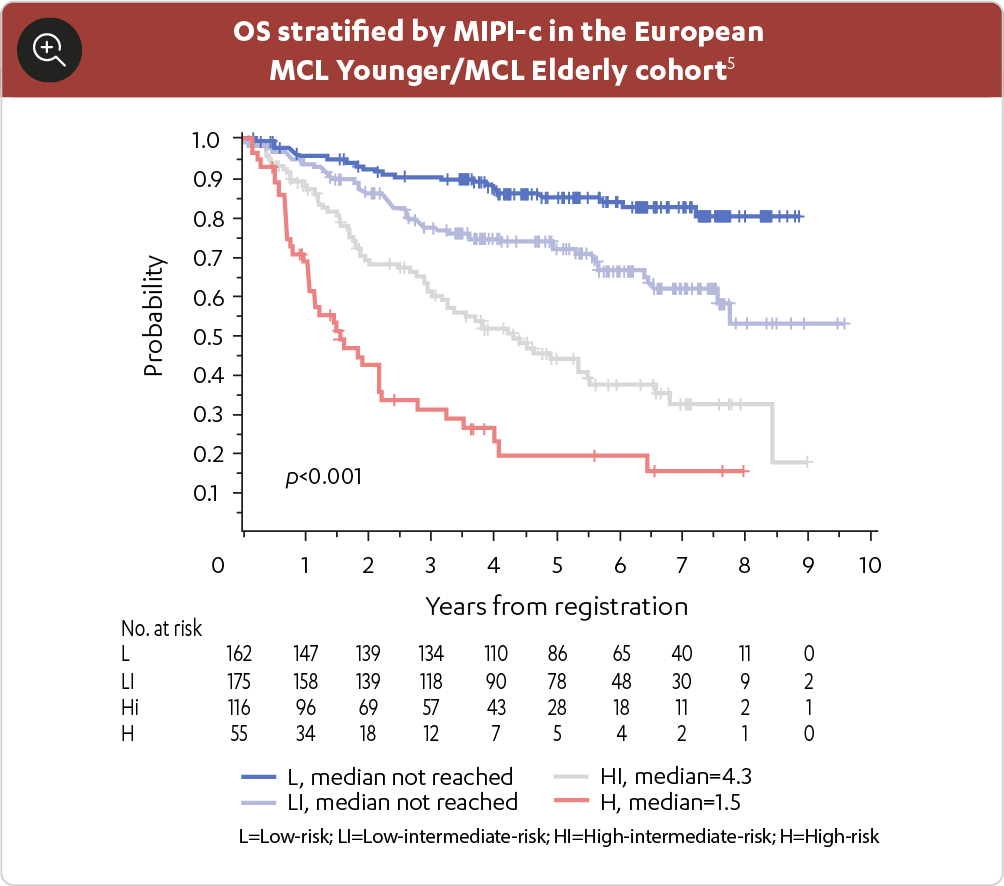
Since treatment may differ depending on the stage of the disease, in-depth evaluation should occur at the initial staging.1,2 The MIPI score is based on several independent prognostic factors at the time of diagnosis, including: age, ECOG performance status, LDH, and white blood cell count – in one study, a high-risk MPI score was associated with poor survival.1,2
For treatment purposes, MCL has been categorized into two major subgroups, these subgroups are now included in the WHO 2016 update of lymphoid malignancies.3
The subgroups of MCL are distinct in clinical presentation and molecular features.3
-
Conventional MCL3
- This is a bulky nodal/extranodal variant with an aggressive disease course
-
Smouldering nodal/extra-nodal and leukemic non-nodal MCL3
- This is seen in 10% to 20% of MCL patients
- In most cases, it is generally associated with indolent disease course and superior outcome
MIPI RISK STRATIFICATION
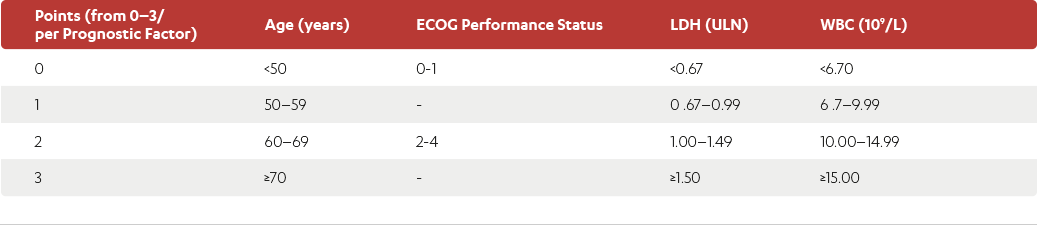
| Points (from 0–3/per Prognostic Factor) | Age (years) | ECOG Performance Status | LDH (ULN) | WBC (109/L) |
|---|---|---|---|---|
| 0 | <50 | 0-1 | <0.67 | <6.70 |
| 1 | 50–59 | 0.67–0.99 | 6.7–9.99 | |
| 2 | 60–69 | 2-4 | 1.00–1.49 | 10.00–14.99 |
| 3 | ≥70 | ≥1.50 | ≥15.00 |
Adapted from Leukemia & Lymphoma Society.
ECOG=Eastern Cooperative Oncology Group; LDH=lactate dehydrogenase; ULN=upper limit of normal; WBC=white
blood cell.
For each prognostic factor, 0–3 points were given to each patient to a maximum of 11.2
- Patients with 0–3 points in total were classified as low-risk, patients with 4−5 points as intermediate-risk, and patients with 6–11 points as high-risk2
- ECOG performance status was weighted with 2 points if patients were unable to work or bedridden (ECOG 2–4)4
- LDH was weighted according to the ratio to the ULN4
- For example an ULN of 240 U/L, the limits were 180, 240 and 360 U/L for low-, intermediate- and high-risk groups, respectively
This risk assessment can help plan the next steps for treatment of MCL by dividing it into:1,3
- Indolent disease – watch and wait
or
- Aggressive disease – active treatment
or
- Relapsed/refractory disease – active treatment
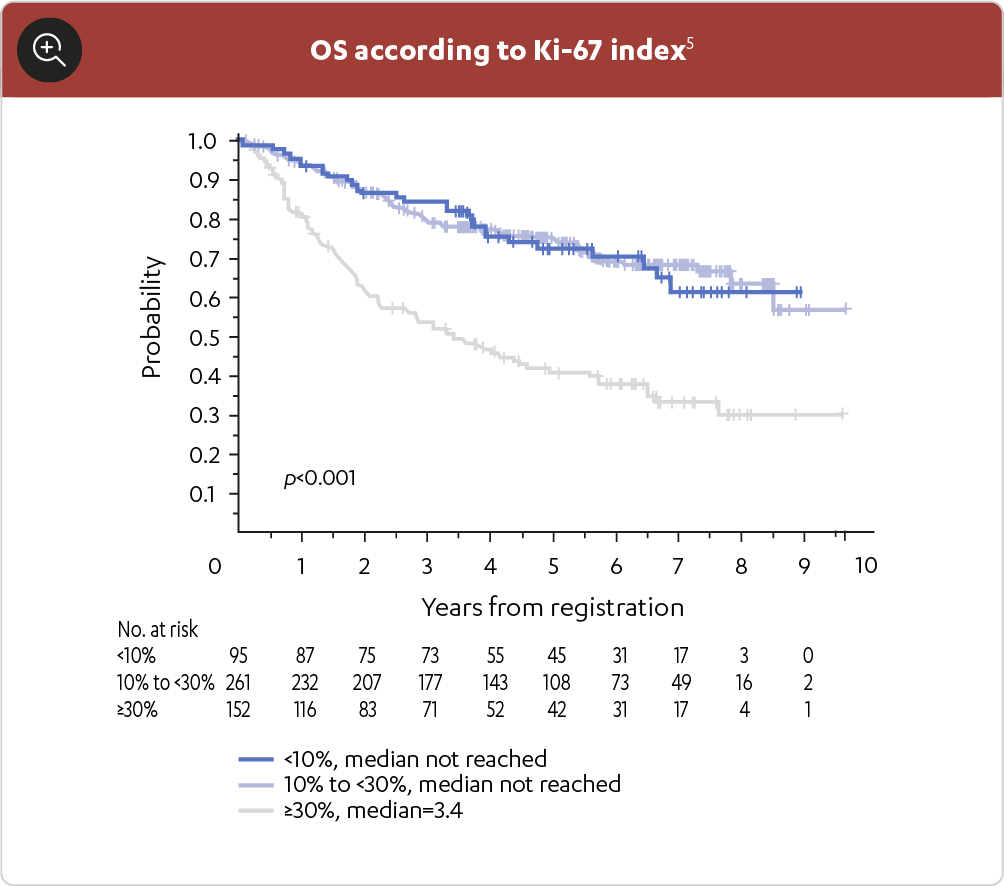
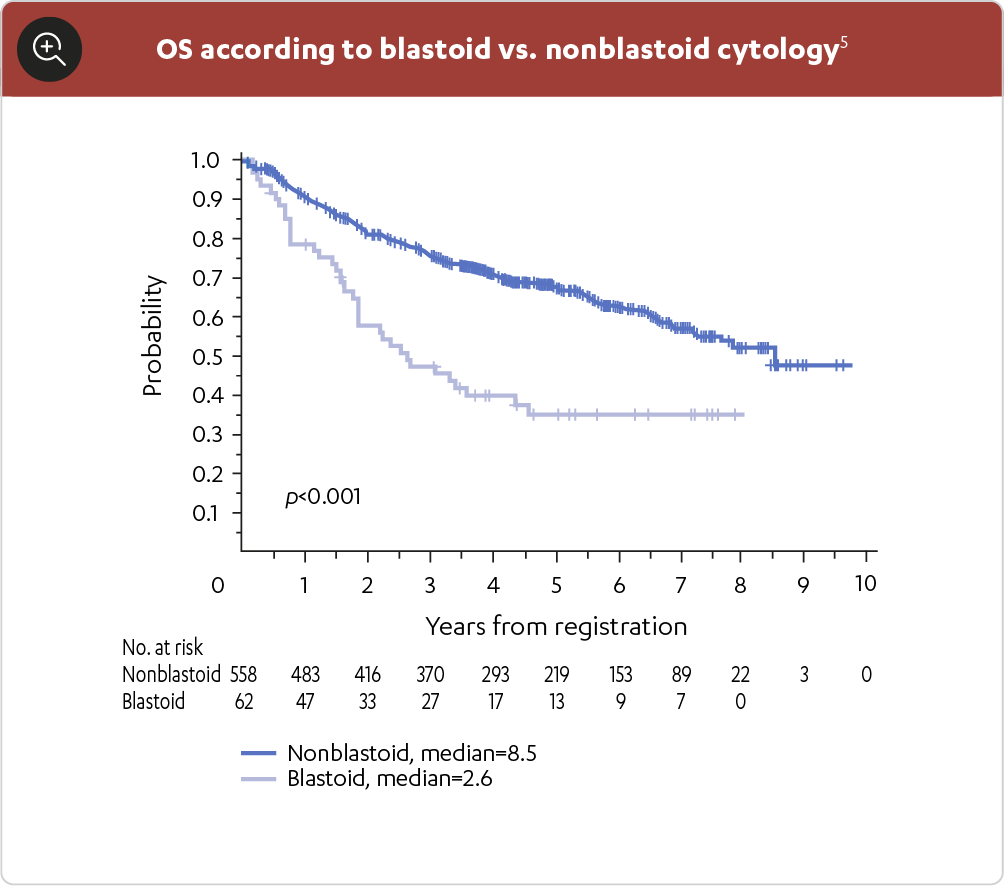
SOME CLINICAL AND MOLECULAR CHARACTERISTICS, SUCH AS BLASTOID MORPHOLOGY, HIGH-RISK MIPI SCORE AND HIGH KI-67, HAVE BEEN SHOWN TO HELP PREDICT OUTCOMES IN MCL PATIENTS1
THE MCL DIAGNOSTIC PROCESS
Staging and prognostic indexes, such as the MIPI, can help inform appropriate treatment strategies based on individual patient risk factors.2
Given the aggressive nature of MCL, approximately 70–80% of patients are symptomatic and require treatment immediately following diagnosis and staging (Table 3).2,3
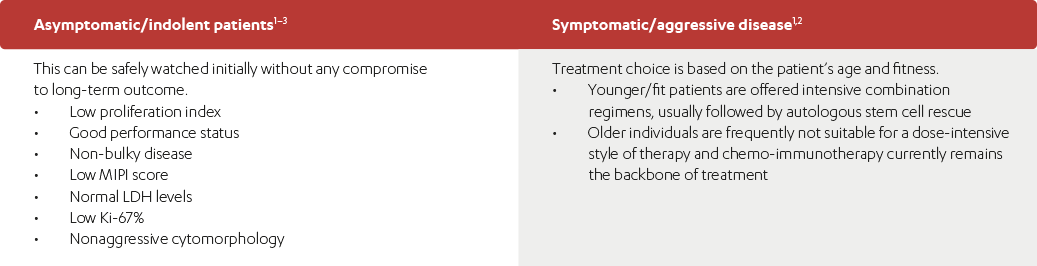
| Asymptomatic/indolent patients: 1–3 | Symptomatic/aggressive disease 1,2 |
|---|---|
This can be safely watched initially without any compromise to long-term outcome.
|
Treatment choice is based on the patient’s age and fitness.
|
References:
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for B-Cell Lymphomas V.1.2022 – March 2, 2022. © National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Accessed March 4, 2022. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
- Leukemia & Lymphoma Society. Mantle cell lymphoma facts. Available at: https://www.llscanada.org/sites/default/files/National/CANADA/Pdf/InfoBooklets/FS4_MCL_2018_FINAL.pdf. Accessed August 24, 2021.
- Jain P and Wang M. Mantle cell lymphoma: 2019 update on the diagnosis, pathogenesis, prognostication, and management. Am J Hematol 2019;94:710–25.
- Hoster E, et al. A new prognostic index (MIPI) for patients with advanced-stage mantle cell lymphoma. Blood 2008;111(2):558–65.
- Hoster E, et al. Prognostic Value of KI-67 Index, Cytology, and Growth Pattern in Mantle-Cell Lymphoma: Results From Randomized Trials of the European Mantle Cell Lymphoma Network. J Clin Oncol 2016;34:1386–94.
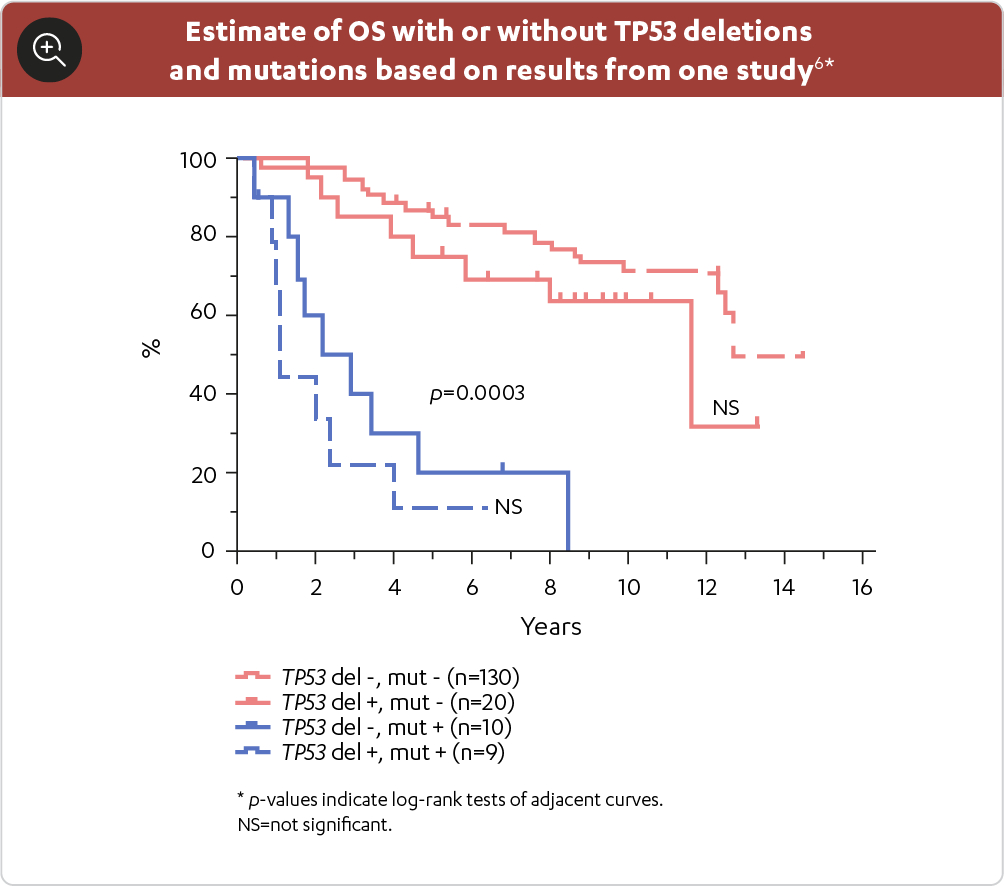
- Eskelund CW. TP53 mutations identify younger mantle cell lymphoma patients who do not benefit from intensive chemoimmunotherapy. Blood 2017;130(1):1903–10.